Type 1 Diabetes and Ramadan Fasting
Ramadan is right around the corner and it’s my favourite month of the year because I get to spend extra time with my family! An important spiritual practice during Ramadan is fasting from dawn until sunset without any food or water.
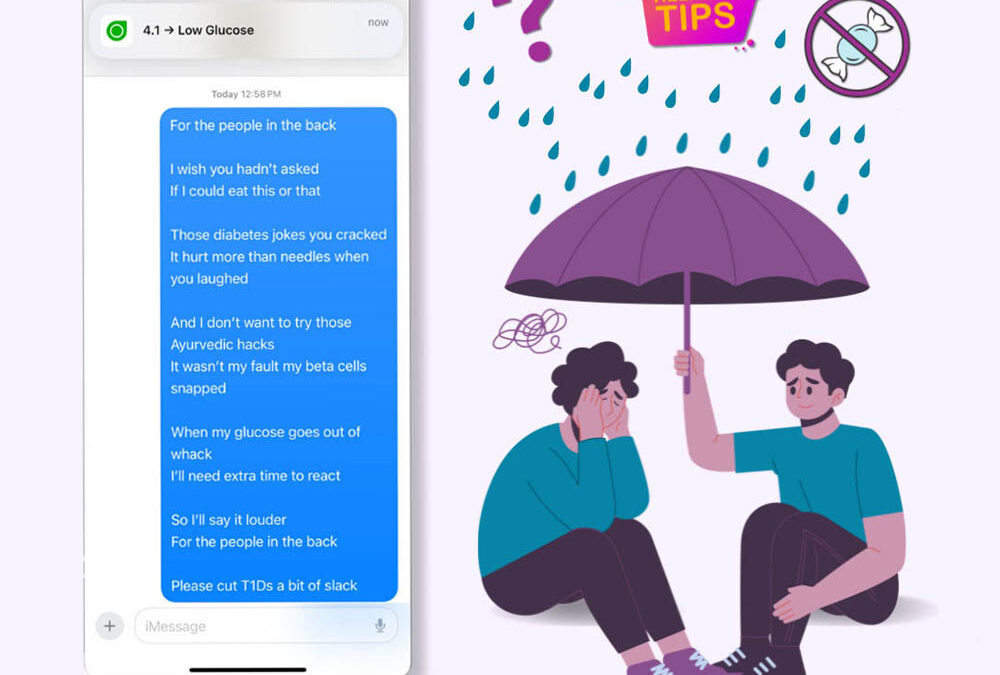
People always ask if everyone has to fast and the short answer is no. I have been Type 1 diabetic for 20 years and I participate through a financial contribution so someone in need can be fed during the 30 days of Ramadan.
The Quran states that fasting is not required if it puts your health at risk. This applies to children, pregnant women and elderly folk as well. The three main risks of fasting with type 1 diabetes include having high glucose (Hyperglycemia), low glucose (Hypoglycemia) and becoming dehydrated, which may be prevented by preparing in advance.
5 Tips for fasting with diabetes in Ramadan:
Many people with diabetes can fast and I have tons of dia-buddies who do every year. Here are a few helpful tips for fasting safely through Ramadan:
- Plan Ahead: Consult your healthcare provider a few months prior to Ramadan to assess if fasting is safe for you. Develop a personalized management plan tailored to your diabetes needs. 1
- Start and break your fast (Iftar) safely: Opt for high-fiber, low-glycemic index foods like whole grains, legumes, fruits, and vegetables during your pre and post fast meals to manage blood sugar levels effectively and slow down on those sweet (yet delicious) dates! Once your fast is over, eat balanced meals at regular times. Drink 2 L of water between sundown and sunrise.2
- Monitor Blood Sugar Levels: Regularly test your blood sugar, especially if you use insulin. This helps catch any fluctuations early and reduces the risk of hypoglycemia during fasting. Checking your blood sugars or using a constant glucose monitor throughout the day won’t break your fast. 3
- Adjust Medications and Timing: Work with your healthcare team to adjust your diabetes medications, including insulin dosage and timing, to accommodate fasting hours safely. 4
- Follow Up Post-Ramadan: Schedule a follow-up appointment with your healthcare provider after Ramadan to address any concerns. This ensures your diabetes management remains on track and minimizes potential complications. 5
Ramadan Mubarak!
“The greatest iftar is to break the fast of apathy, with the feast of affection” ~ Abhijit Naskar
9 Tips for breaking the fast on Eid:
Breaking the fast, especially during Ramadan, is a significant moment for individuals with type 1 diabetes. Here are some best practices specifically for breaking the fast during Ramadan or any fasting period:
- Monitor Blood Sugar Levels: Check your blood sugar levels before breaking your fast. This will help you determine whether your blood sugar is within a safe range or if you need to take action to bring it to a safe level before eating.
- Choose Nutrient-Dense Foods: Opt for foods that are nutrient-dense and provide a good balance of carbohydrates, protein, and healthy fats. This can help prevent rapid spikes in blood sugar levels after breaking the fast. Examples include whole grains, lean proteins, vegetables, and healthy fats like avocados or nuts.
- Start with Water and Dates: Traditionally, many Muslims break their fast with dates and water. Dates provide a quick source of natural sugars to raise blood sugar levels, while water helps with hydration. This can be followed by a balanced meal.
- Control Portion Sizes: Be mindful of portion sizes when breaking your fast. Eating too much too quickly can cause blood sugar levels to spike. Start with smaller portions and eat slowly, giving your body time to process the food.
- Avoid Sugary Foods and Drinks: While it may be tempting to indulge in sweets and sugary drinks after fasting, these can cause rapid fluctuations in blood sugar levels. Opt for healthier alternatives and limit your intake of sugary foods and beverages.
- Space Out Meals and Snacks: If possible, try to space out your meals and snacks throughout the evening and night to prevent large fluctuations in blood sugar levels. This can help keep your blood sugar levels more stable.
- Stay Active: Engage in light physical activity after breaking your fast, such as taking a short walk. This can help improve insulin sensitivity and aid in digestion, which may help regulate blood sugar levels.
- Consult with a Healthcare Provider: If you’re unsure about how fasting will affect your diabetes management or if you have any concerns, consult with your healthcare provider before Ramadan begins. They can provide personalized guidance and advice based on your individual health needs.
- Listen to Your Body: Pay attention to how your body responds to fasting and breaking the fast. If you experience symptoms of hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar), take appropriate action and seek medical attention if necessary.
By following these best practices, individuals with type 1 diabetes can effectively manage their condition while participating in fasting during Ramadan or other religious observances. It’s essential to prioritize health and safety while honoring religious traditions.
Helpful Resources
General information about Ramadan 2024: https://www.islamicreliefcanada.org/our-work/ramadan
Statement for People With Diabetes Who Fast During Ramadan: View here >
Sources:
1, 4, 5 “Fasting at Ramadan and Diabetes: Summary”, Diabetes Canada, Retrieved 7 March 2024. <https://www.diabetes.ca/advocacy—policies/our-policy-positions/fasting-at-ramadan-and-diabetes–summary>
2 “How to Observe Ramadan Safely With Type 1 Diabetes”, Type 1 BETTER, Retrieved 7 March 2024. <https://type1better.com/en/how-to-observe-ramadan-safely-with-type-1-diabetes/>
3 “Diabetes among Muslims during Ramadan: A narrative review”, NIH, Retrieved 07 March 2024. <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10507567/>

About the Author
My name is Amal Bashir and I’ve been living with Type 1 Diabetes since I was 8 years old and received a Diabetes Hope Scholarship in 2013. I’ve been working in the tech industry since 2018 and I have been a visual artist for most of my life. I have a big personality and an even bigger heart!













0 Comments